Can cardiopulmonary exercise test results predict the length of critical care stay in patients undergoing simultaneous kidney pancreas transplant?
Lucija Kovacic1, Mortimer Kelleher1, Helen Usher1, Shaun Baxter3, Aaron Hui2, Andrew Sutherland2, Euan Thomson1.
1Department of Anaesthesia, Royal Infirmary of Edinburgh, Edinburgh, United Kingdom; 2Department of Transplant surgery, Royal Infirmary of Edinburgh, Edinburgh, United Kingdom; 3Department of Respiratory physiology, Royal Infirmary of Edinburgh, Edinburgh, United Kingdom
Introduction: Cardiopulmonary exercise testing (CPEX) has been able to accurately predict patient mortality, graft outcomes and length of hospital stay in some solid organ transplants (such as liver and kidney), however, no study has so far been published that has examined the ability of CPEX to predict non-cardiac outcomes in patients undergoing simultaneous kidney pancreas (SKP) transplant. We aimed to determine the ability of CPEX to predict outcomes in SKP transplant patients.
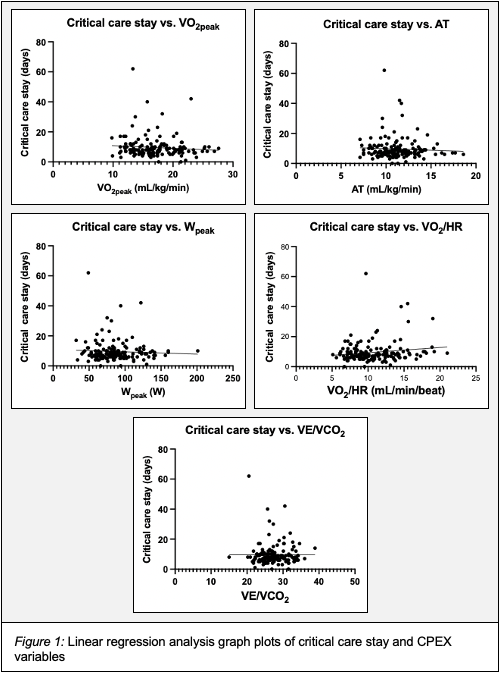
Methods: A single centre retrospective analysis of patients that underwent SKP transplant at Edinburgh Transplant Centre between 2011 and 2020 was carried out. Patients were included if they had performed at least one CPEX prior to surgery and if their results were available. Five CPEX variables were included in the study (peak oxygen consumption (VO2peak), anaerobic threshold (AT), peak workload (Wpeak), oxygen pulse (VO2/HR), ventilatory equivalent for carbon dioxide (VE/VCO2)). The primary outcome was the length of postoperative critical care unit stay. Additional data was collected for length of hospitalisation, mortality and graft outcomes.
Results: 156 patients underwent SKP transplant at Edinburgh Transplant Centre in the 9-year period. 8 patients were excluded from the final analysis: 4 patients as they did not perform a CPEX and 4 as they had incomplete data available. Mean length of stay in critical care was 9.59 days (SD: 7.47 days). Univariate analysis found no significant association between CPEX and length of critical care stay.
To correct for cofounders, stepwise linear regression with backwards elimination was performed. It identified five other recipient characteristics that had a significant influence on the length of critical care stay (age: p=0.028, BMI: p=0.049, pre-transplant CVA and blindness: p=0.0093 and p=0.036, length of pre-transplant dialysis: p=0.007). Average length of hospitalisation was 19.27 days (SD: 11.67 days). When comparing CPEX results for other secondary outcomes (mortality, rejection episodes and insulin independence), there was no significant between-group difference in CPEX variables.
Conclusion: In our population, CPEX had limited ability at predicting the length of critical care and hospital stay, and did not predict mortality or graft outcomes post-transplant. A possible explanation for this is exclusion of patients with poor CPEX results from being listed for SKP transplant which reduces the sensitivity of CPEX to predict length of critical care stay. Future studies are needed to further evaluate this relationship.