Safety of islet transplantation in the preperitoneal space in addition to intraportal infusion in clinical total pancreatectomy with islet autotransplantation
Nicholas Onaca1, Kenjiro Kumano1, Jordan Mattke1, Carly Darden1, Srividya Vasu1, Yang Liu1, Michael Lawrence1, Mariagrazia Coluzzi1, Giuliano Testa1, Amar Gupta1, Ernest Beecherl1, Bashoo Naziruddin1.
1Transplant, Baylor Simmons Transplant Institute, Dallas, TX, United States
Introduction: Total pancreatectomy and intraportal islet autotransplantation (TPIAT) is an effective treatment for patients with refractory chronic pancreatitis. Large volume islet preparations cannot always be infused fully intraportally due to rise in portal vein (PV) pressure and risk of PV thrombosis. We previously showed that dissected preperitoneal pouch (preperitoneal space) can serve as an extrahepatic islet transplant site with long-term graft function in syngeneic mouse model. Here, we evaluated the safety of combined sites of intrahepatic and preperitoneal space in clinical TPIAT and analyzed the outcome.
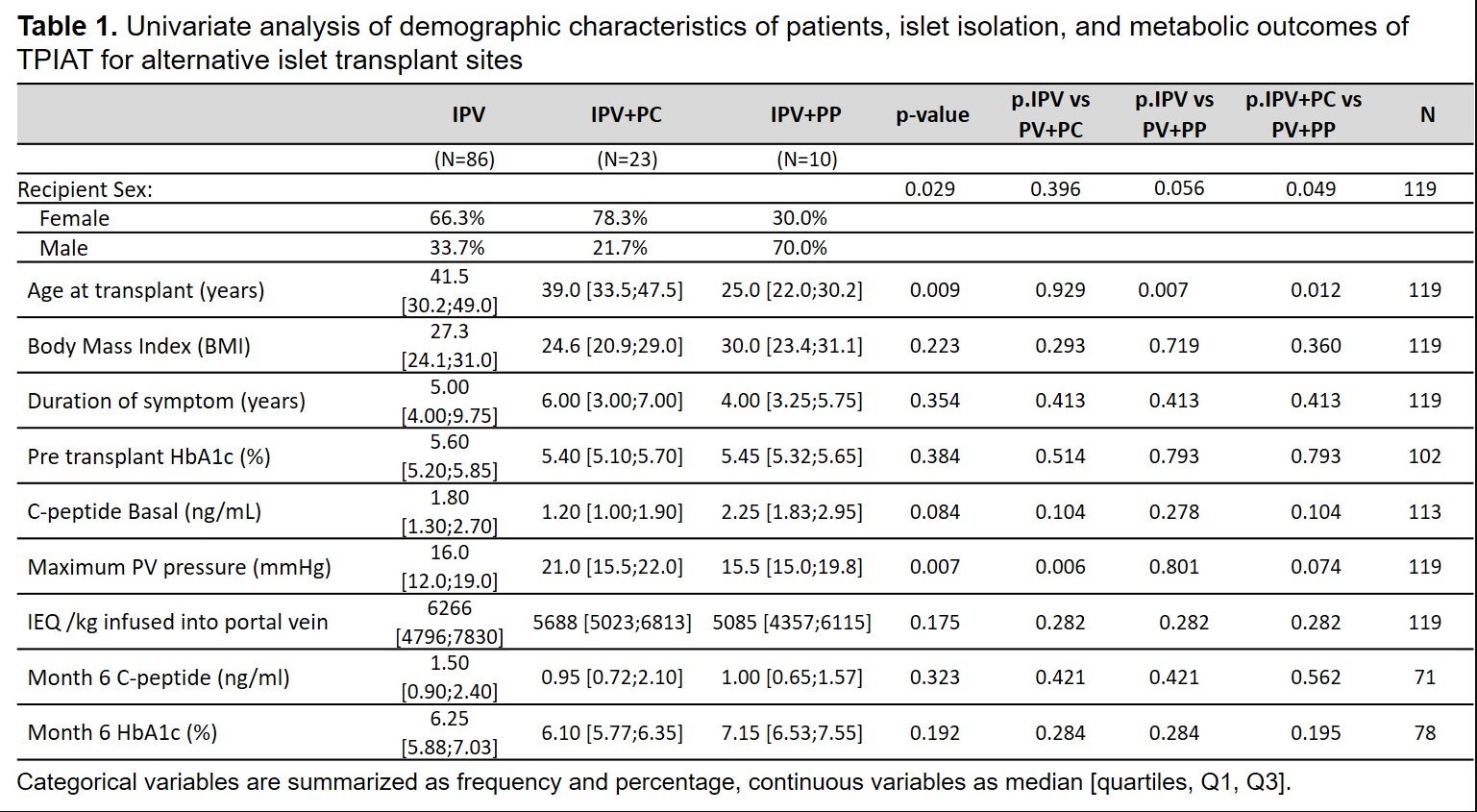
Method: Between 2019 and 2020, patients underwent TPAIT using a combined intraportal and preperitoneal pouch technique (IPV+PP) if the infused intraportal islet mass was >4,000 islet equivalents per kg (IEQ/kg) and PV pressure was > 20mmHg during infusion. Patients were monitored for complications, and metabolic outcome was assessed and compared with controls who received only intraportally transplanted islets (IPV) or combined intraportal and into the peritoneal cavity (IPV+PC).
Results: Ten patients underwent TPIAT into the PV and preperitoneal pouch. Baseline demographics (age, sex, BMI, pretransplant C-peptide and HbA1c, duration of symptoms), PV pressure, islet mass by IEQ/kg of each group are shown in Figure 1. There were no serious post-operative complications in the IPV+PP group during the first post-transplant admission. At 6 months after TPIAT, there were no significant differences in glycemic control or graft function among three groups (Figure 1).
Conclusion: The preperitoneal space is an alternative supplemental islet infusion site in patients who do not tolerate a full intraportal islet infusion. It is safe, easily accessible and it tolerates large volume islet preparations. Further studies are needed on a larger number of patients to validate our results.