Ultrastructural assessment of the associations of obesity and established diabetes in human pancreata
Nicola Dyson1, Nicole Kattner1, Serena Carey1, Minna Honkanen-Scott1, Bethany Hunter1, Tracey Davey2, James AM Shaw1,3, William E. Scott III1.
1Translational and Clinical Research Institute, Newcastle University, Newcastle upon Tyne, United Kingdom; 2Electron Microscopy Research Services, Newcastle University, Newcastle upon Tyne, United Kingdom; 3Institute of Transplantation, Freeman Hospital, Newcastle upon Tyne Hospitals NHS Foundation Trust, Newcastle upon Tyne, United Kingdom
Introduction: The increase in global prevalence of Type 2 diabetes (T2D) and associated complications of this condition such as neuropathy and nephropathy present considerable challenges for health care systems worldwide. T2D is often linked with obesity and characterised by β-cell dysfunction and insulin resistance. The potential association between intracellular lipid accumulation and β-cell stress and dysfunction has not been researched in detail in intact human pancreas. This study analysed the impact of obesity and T2D on the ultrastructure of cell organelles as well as lipid and lipofuscin accumulation using transmission electron microscopy (TEM).
Method: Biopsies of human pancreata were collected in a standardised manner as part of the Quality in Organ Donation (QUOD) Expand project, processed, and imaged with TEM as previously described (Kattner et al 2020). A cohort of 15 donors including five without diabetes with body mass index (BMI) <30 kg/m2, five without diabetes with BMI>30 kg/m2 and five with T2D were analysed. Donors were matched for age, gender, and cold ischaemia time. Acute impact on acinar and endocrine cells was assessed using the novel Newcastle Pancreatic Acinar/Endocrine Scoring Systems (NPASS/NPESS). Additionally, measurement of intracellular lipid and lipofuscin accumulation was carried out using ImageJ.
Results: NPASS/NPESS scores were comparable to those with BMI <30kg/m2 in the groups with high BMI/T2D. A trend towards increased endocrine lipid and decreased exocrine lipid accumulation was observed in high BMI and T2D donors relative to the lower BMI group (Figure 1), reaching significance for exocrine lipid in the donors with T2D (p=0.003). Lipofuscin accumulation was comparable between all groups. Ratios of α- and β-cell number were comparable between the three groups, whereas β-cell area was significantly decreased with higher BMI (p=0.027) and lowest with T2D (p<0.0001)(Figure 2). A sub-analysis of all β-cells showed significantly increased lipofuscin accumulation compared to α-cells (p<0.0001). In addition, a heterogeneous endocrine cell type was observed containing granules of both β- and α-type morphological appearance. These heterogeneous cells exhibited increased intra-cellular lipid (p=0.025) with lipofuscin greater than α-cells and less than β-cells (p=0.046)(Figure 2).
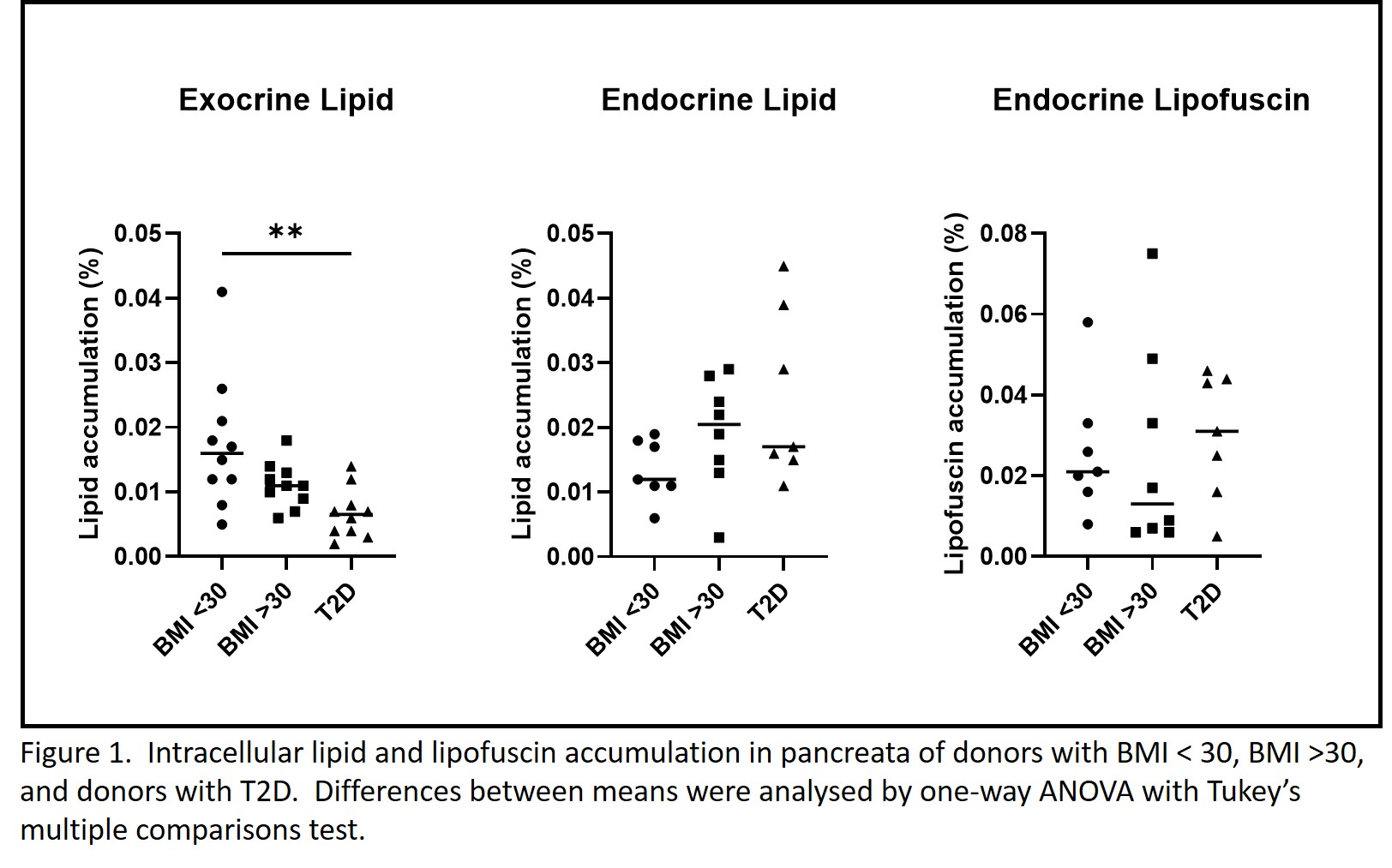
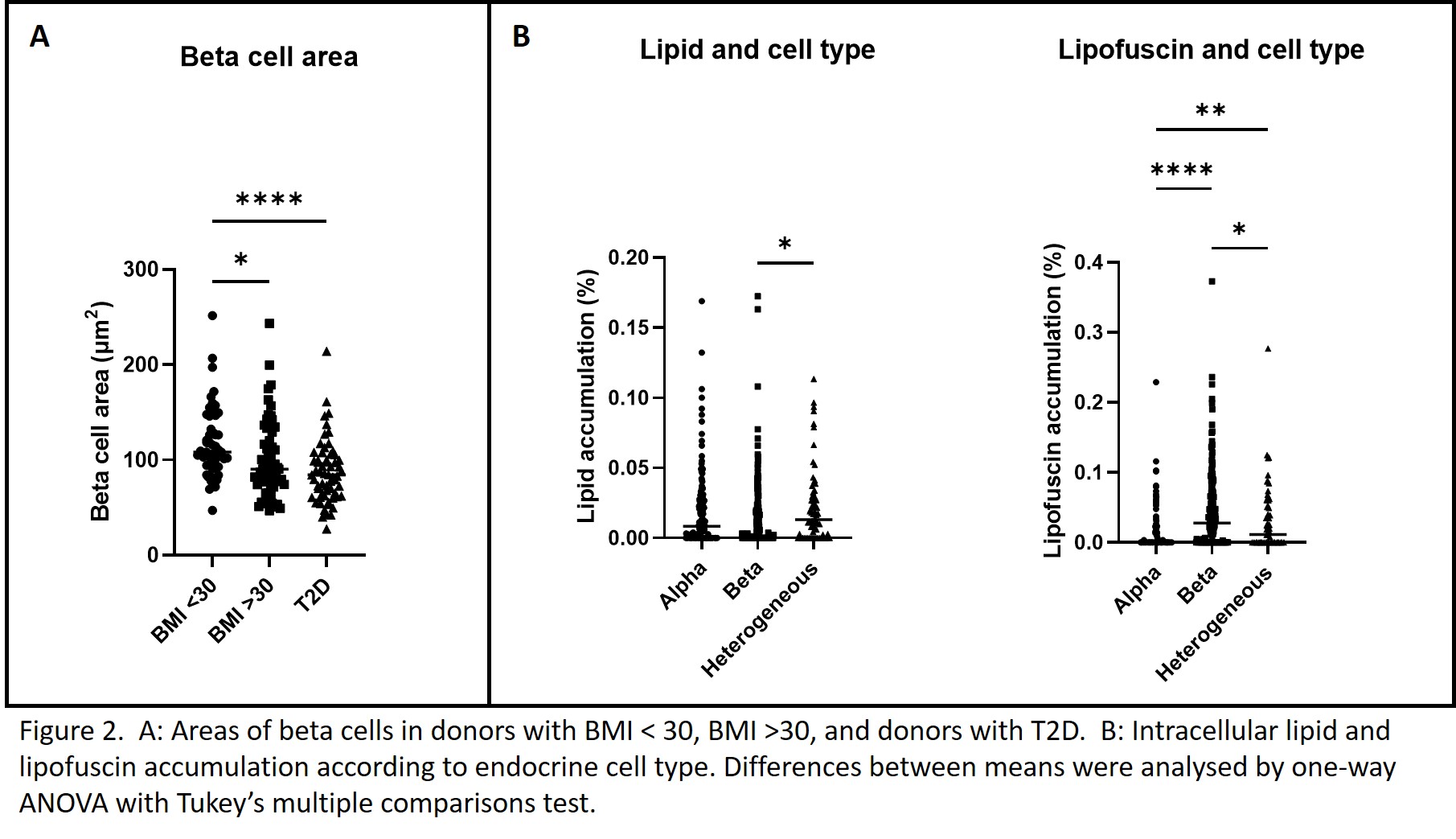
Discussion: Obesity and T2D had little acute impact on the sub-cellular ultrastructure of pancreatic cells, but were associated with alterations in intracellular lipid accumulation, with no evidence of increased β-cell turn-over (i.e. no reduction in lipofuscin accumulation). Heterogeneous cells suggestive of a transitional phenotype between α- and β-cells appeared to be of intermediate ‘age’ (lipofuscin) and more prone to lipid accumulation. Further understanding of the mechanisms leading to the changes observed here may deepen our understanding of islet dysfunction in T2D and lead to new therapeutic interventions.
MRC (Quality and Safety in Organ Donation Tissue Bank - Expansion to include Pancreas/Islets, Heart and Lungs) (MR/R014132/1) . National Institute for Health Research Newcastle Biomedical Research Centre. National Institute for Health Research Blood and Transplant Research Unit (NIHR BTRU) in Organ Donation and Transplantation. BBSRC grant BB/R013942/1. EPSRC CL086 studentship 150648356 supported by an EPSRC RiHN Feasibility Studies (UK) (EP/M017559/1).