Does Pre-transplant Hypertension Affect the Outcomes of Total Pancreatectomy with Islet Auto-transplantation?
Prathab Balaji Saravanan1, Jagan Kalivarathan1, Marlon F. Levy1, Mazhar Kanak1.
1Hume Lee Islet Transplant Lab, Department of Surgery, VCU Health, Richmond, VA, United States
Aim: Hypertension is a common health concern worldwide, which is often accompanied with comorbidities. We have observed an increased incidence of hypertension (>30%) in chronic pancreatitis patients at our center. The association between hypertension and the outcomes of TPIAT has not been previously studied. This study aims to investigate if pre-op hypertension affects the metabolic outcomes of TPIAT.
Methods: We retrospectively analyzed the demographics, isolation outcomes, and infusion status along with the metabolic outcomes pre and post-transplant, in 21 TPIAT patients. The recipients were divided into two groups namely hypertensive (HT), and non-hypertensive (NHT). Data analyses were performed using GraphPad Prism 7. The difference of the means and variances between the groups were tested by Student’ t-test and f-test respectively.
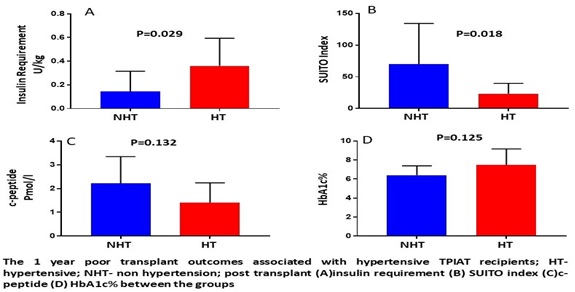
Results: Out of 21 TPIAT patients, 8 (38%) had pre-op hypertension or were on hypertension medication before the start of the TPIAT procedure. There was no significant difference in the IEQ/g of the pancreas (5688±631.4 vs 4416±836.8 IEQ/g of the pancreas, p=0.274) and the islet transplant dose (5442±714 vs 4074±974 IEQ/kg of the recipient, p=0.244) between the NHT and the HT group. There is no difference in the patient’s characteristics including BMI, disease duration, pain and pancreas fibrosis score, pretransplant recipients HbA1c% and c-peptide levels between the HT and NHT group. The statistical analysis showed, TPIAT patients with pre-OP HT required a significantly higher amount of exogenous insulin posttransplant (0.36±0.09 vs 0.14±0.04 p=0.029) and also, achieved poor beta-cell function as calculated by the SUITO index (23.36±7.3 vs 70.24±18.4, p=0.018) compared to the NHT group after 1-year post-TPIAT (fig:A&B). There was no significant difference in the post-transplant c-peptide (1.4±0.3 vs 2.2±1.4, p=0.132), and HbA1c (7.46±0.7 vs 6.4±0.2, p=0.125) compared to the NHT group (fig:C&D).
Conclusion: The study results suggest that CP patients with hypertension may have poor beta-cell functional capability compared to non-hypertension patients. However, further investigation is warranted as the sample size is not strong enough to conclude. We will investigate more patients in this study and validate our findings with more robust statistical outcomes.