The presence of donor-specific antibodies around the time of pancreas graft biopsy with rejection is associated with an increased risk of graft failure
Sandesh Parajuli1, Arjang Djamali1, Didier Mandelbrot1, Fahad Aziz1, Nancy Radke2, Dixon Kaufman2, Jon Odorico2.
1Medicine, University of Wisconsin-Madison, Madison, WI, United States; 2Transplant Surgery, University of Wisconsin-Madison, Madison, WI, United States
Introduction: Donor-specific antibodies (DSA) against human leukocyte antigen (HLA) are an important biomarker predicting graft injury, rejection (Rej), and failure in various solid organ transplant recipients. However, the impact of DSA with or without Rej among pancreas transplant recipients (PTRs) is unknown.
Method: In this study, we included all PTRs who had undergone either simultaneous pancreas-kidney or solitary pancreas transplant at our center between 2005 and 2020, with pancreas allograft biopsy before 03/2021, and with DSA checked within 15 days of the biopsy. Among PTRs with multiple biopsies during the study period, the first index biopsy was used to analyze the data. Pancreas biopsies at the time of implant or explant were excluded, as were biopsies with no pancreas tissue present. PTRs were divided into four groups based on the biopsy findings on the index biopsy and DSA status as Rej-/DSA-; Rej+/DSA-; Rej-/DSA+ and Rej+/DSA+.
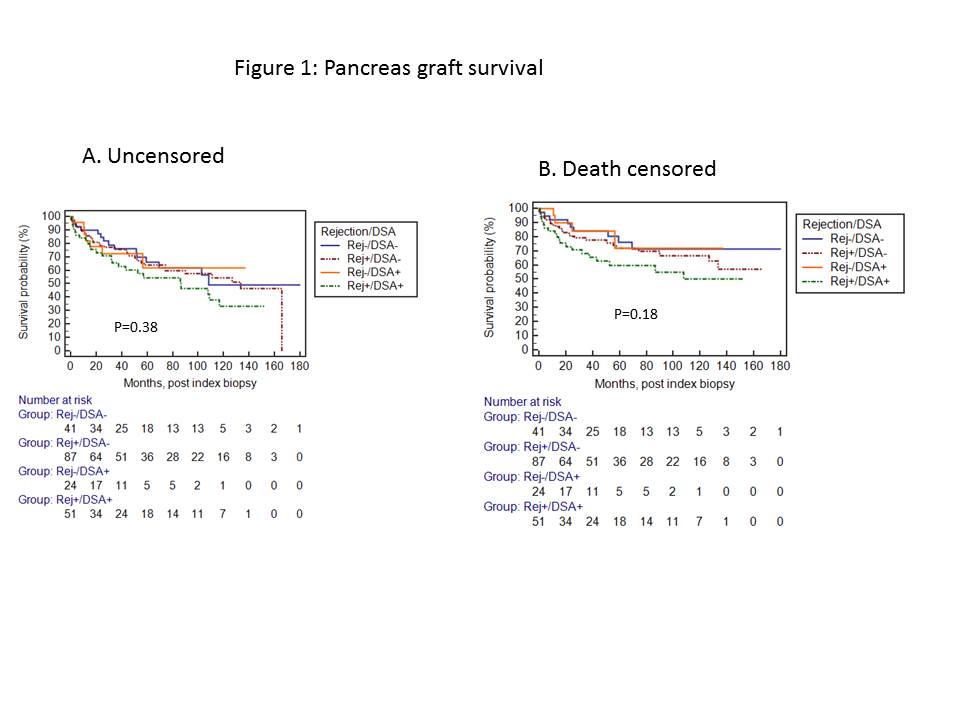
Results: A total of 352 pancreas allograft biopsies were performed in 203 PTRs during the study period. Of these, 203 PTRs, 41 were in Rej-/DSA- ; 87 Rej+/DSA-; 24 Rej-/DSA+; and 51 Rej+/DSA+. Most of the baseline characteristics were similar between the groups, except PTRs in Rej-/DSA+ and Rej+/DSA+ were relatively younger, with a mean age of 39 compared to 43 for the other two groups. The mean interval from transplant to index biopsy was not statistically different between the four groups. The most common rejection was TCMR, however, AMR was more prevalent in the Rej+/DSA+ group. In addition, DSA against class II HLA was more prevalent in the DSA+/Rej + group. There was no statistical difference in the mean post index biopsy follow-up. At last follow up, the rate of death censored graft failure (DCGF) for Rej-/DSA- was 22%, 29% in Rej+/DSA-; 17% in Rej-/DSA+ and 39% in Rej+/DSA+. Although not statistically significant, there was a trend towards inferior pancreas graft survival in Rej+/DSA+ group by unadjusted K-M survival analysis (Figure 1).
In multivariable analysis compared to Rej-/DSA-, Rej+/DSA+ was significantly associated with DCGF (HR: 2.25, 95% CI: 1.02 to 4.97; p=0.04), however Rej+/DSA- was not (HR: 1.40; 95% CI: 0.65 to 3.0; p=0.39).
Conclusions: PTRs with pancreas allograft rejection in the presence of DSA have an increased risk of DCGF, and may warrant particularly aggressive management.