Effect of HLA Matching on Long Term Islet Allograft Function
Joana Lemos1, Virginia Fuenmayor1, David Baidal1, Raffaella Poggioli1, Carmen Chavez1, Ana Alvarez1, Camillo Ricordi1, Rodolfo Alejandro1.
1Clinical Cell Transplant Program, Diabetes Research Institute - University of Miami, Miami, FL, United States
Introduction: Islet Cell Transplantation (ITx) is an effective therapeutic approach for selected patients with type 1 diabetes affected by hypoglycemia unawareness and severe hypoglycemia events. In whole organ transplantation, HLA mismatching has been shown to negatively impact transplant outcomes. We aimed to determine whether HLA matching has an impact on islet allograft survival.
Methods: A retrospective cohort study was conducted in 56 ITx patients followed at our institution between 2000 and 2020. Fifty-three subjects underwent intrahepatic ITx (46 ITx alone and 7 islets after kidney) whereas 3 subjects received islets via a laparoscopic omental approach. Immunosuppression treatment was dependent on the clinical transplant protocol.
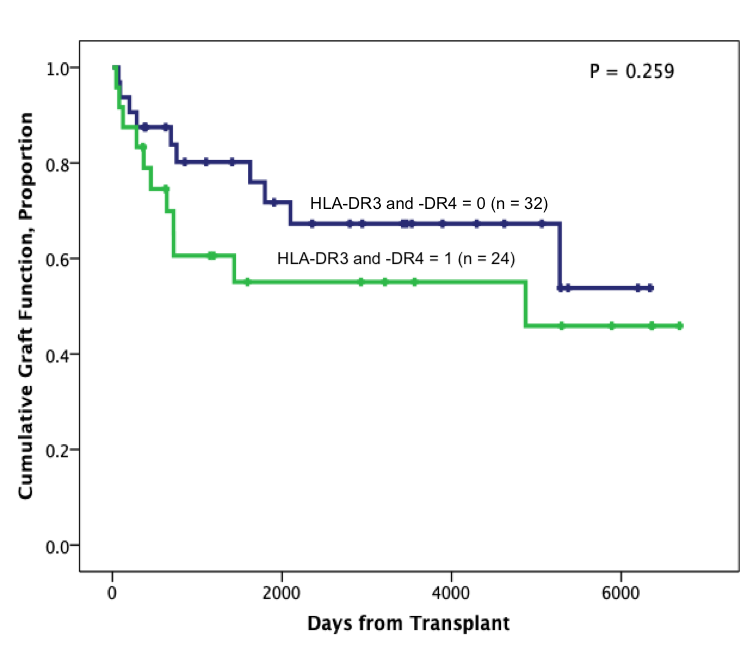
Results: Patients were aged 43.0 ± 8.0 years, and 64.3% (n= 36) of the recipients were female. Diabetes duration was 28.6 ± 11.6 years. HLA data were restricted to -A, -B, and -DR loci. Matching for HLA-DR3 and -DR4 showed a shorter duration of graft function.
The analysis of the time of graft function for combined loci HLA-A, -B, and –DR excluding subjects who matched for HLA-DR3 and -DR4 showed that subjects with ≥1 HLA-A, -B, and –DR matching have longer graft function (P=0.032).
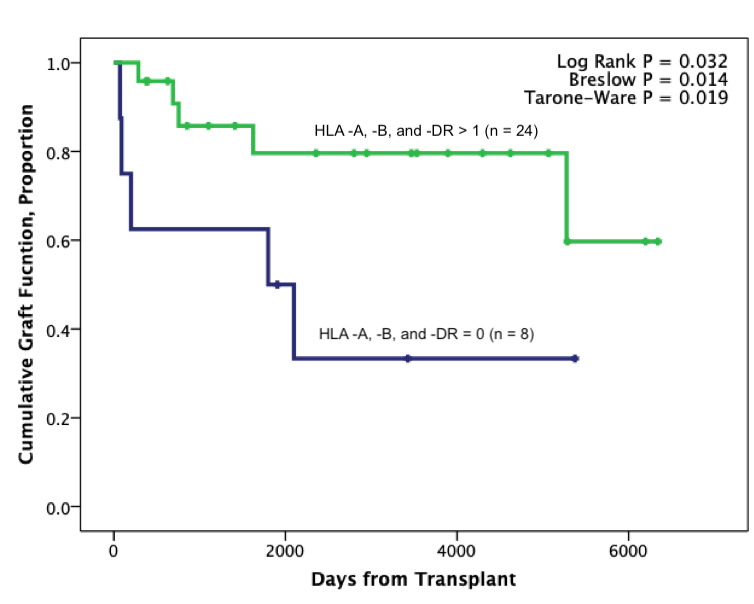
Multivariable Cox proportional hazards regression analysis adjusted for the number of donors, recipient age, T-cell depletion immunosuppression induction, and GLP1 RA and/or DPP4i use showed that ≥1 matching for HLA -A, -B, and -DR decreased the risk of graft failure compared to zero matching group (HR 0.075 [95% CI 0.011–0.497]; P = 0.007).
Conclusion: Our data suggest that HLA-A, -B, and -DR matching (excluding HLA-DR3 and -DR4 matching) is associated with improved islet allograft survival. HLA matching may improve long-term graft function outcomes. Prospective studies with a larger sample size are warranted to validate our findings.
This work was supported by NIH grants R01 DK55347, R01 DK056953, R01 DK025802, DK070460, R01DK55347, U42 RR016603, M01RR16587, UL1TR000460; the Miami Clinical and Translational Science Institute (CTSI) from the National Center for Advancing Translational Sciences and the National Institute on Minority Health and Health Disparities; the Juvenile Diabetes Research Foundation International 4-200-946, 4-2004-361, 17-2012-361, 3-SRA-2017-347-M-B; the State of Florida; and the Diabetes Research Institute Foundation.