Prolonged islet allograft function in patients with type 1 diabetes after islet transplantation is associated with female sex of donors and recipients
Joana Lemos1, David Baidal1,3, Raffaella Poggioli1, Virginia Fuenmayor1, Ana Alvarez1, Elina Linetsky1, Franck Mauvais-Jarvis4,5,6, Camillo Ricordi1,2, Rodolfo Alejandro1,3.
1Clinical Cell Transplant Program, Diabetes Research Institute - University of Miami, Miami, FL, United States; 2Division of Cellular Transplantation, Department of Surgery, University of Miami, Miami, FL, United States; 3Division of Endocrinology, Diabetes and Metabolism, Department of Medicine, University of Miami, Miami, FL, United States; 4Section of Endocrinology and Metabolism, Deming Department of Medicine, Tulane University School of Medicine, New Orleans, LA, United States; 5Tulane Center of Excellence in Sex Based Biology & Medicine, New Orleans, LA, United States; 6Southeast Louisiana Veterans Health Care System, New Orleans, LA, United States
Introduction: Islet transplantation (ITx) has proved to be effective in preventing severe hypoglycemia and improving metabolic control in selected subjects with T1D. Long-term graft function remains a challenge. Estrogens have been shown to protect β-cells from metabolic stresses and improve revascularization of transplanted human islets in the mouse. We aimed to evaluate the influence of sex in allograft survival of ITx recipients.
Methods: We analyzed a retrospective cohort of ITx recipients (n=56) followed for up to 20 years. Allograft failure was defined as a stimulated C-peptide <0.3 ng/ml during a mixed-meal tolerance test. Subjects were divided into recipients of at least one female donor (Group 1) and recipients of male donors only (Group 2).
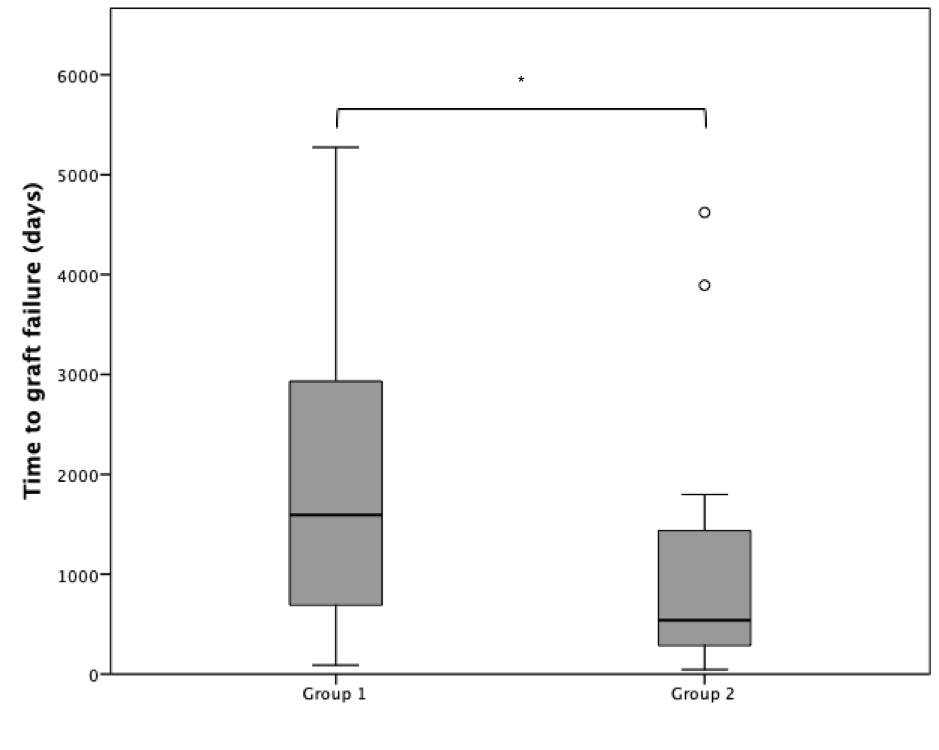
Results: Group 1 subjects (n=25) were aged 41.5 ± 8.4 years and Group 2 subjects (n=22) 45.9 ± 7.3 years (P= 0.062). Female recipient frequency was 44.8% (n=13) in Group 1 and 55.2% (n=16) in Group 2 (P=0.145). Group 2 developed graft failure earlier than Group 1 [680 (286 – 1624) vs. 1906 (756 – 3256) days, P= 0.038, Figure 1].
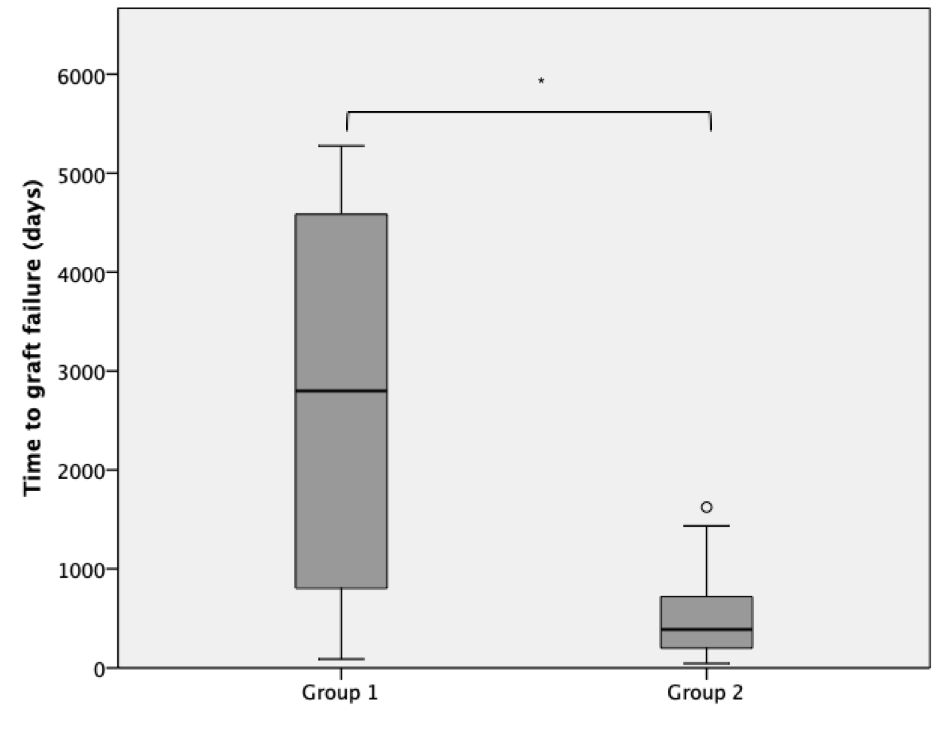
We performed additional analyses on female recipients only from each group (Group 1, n= 16, Group 2, n=20). Female recipients in Group 1 exhibited prolonged allograft function compared to Group 2, after adjustment for recipient age, and GLP 1 receptor agonists use (OR: 28.6, CI: 1.3 – 619.1; P < 0.05; Figure 2).
Conclusion: Recipients of islets from at least one female donor exhibited prolonged graft survival compared to recipients of islets from exclusively male donors. In addition, female recipients exhibited prolonged survival compared to male recipients following ITx of at least one female donor.