
Improving microcirculation to transplanted human islets utilizing peri-pancreatic microvascular fragments
Appakalai Natarajan Balamurugan1, Samaga Krishna Kumar1, Siddharth Narayanan1.
1Department of Peadiatrics, Center for Clinical and Translational Research, Nationwide Childrens Hospital, and Ohio State University, Columbus, OH, United States
Transplanted islets undergo cell death immediately after transplantation due to poor blood supply to inner core. Islet isolation process severs existing peri-islet vascular connections. Stimulation of intraislet endothelial cells to form peri-islet vessels (PIV’s) in vitro prior to transplantation may accelerate post-implant islet revascularization. Intra-pancreatic microvascular fragments are known to create microvascular networks and release angiogenic tropic factors. However, for the first time, we evaluated the effect peripancreatic fat-derived microvascular fragments (PPMVF) cells on PIV formation in a 3D-culture system.
Human islets were isolated from brain-dead donor pancreases (n=15) according to our laboratory protocol. Peripancreatic fat was collected around the pancreas and PPMVF cells were isolated using MVF cell isolation method.
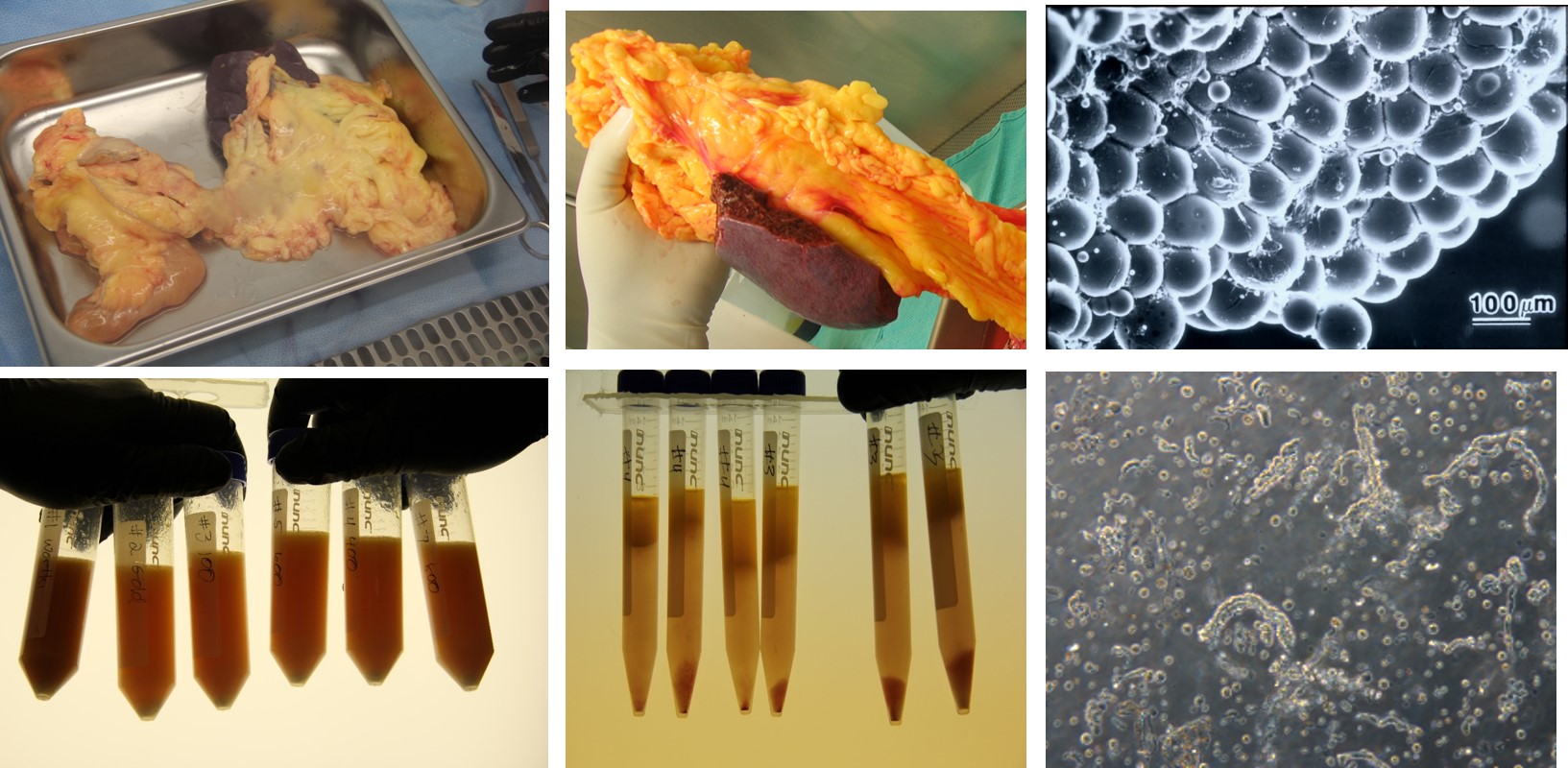
Isolated human islets were cultured in a 3D collagen gel (rat tail collagen-1) for 14 days with PPMVF cells (250,000 cells). Confocal microscopy and Time-lapse microscopy (Cytation 5) was used to monitor islet-derived PIV growth every day for 14 days.
Human islets co-cultured with PPMVF cells induced cellular sprouting within 7 days. Many of these sprouts appeared to be PIV since they resembled a vasculature that arose from the islets. Our labeling indicated that several of these sprouts were endothelial. Intraislet endothelial cells were stained with UEA-1 and we speculate these cells were the source of the peri-islet sprouts. 3D-cultured islets maintained >90% cellular viability after 14 days, whereas 2D-cultured islets displayed disintegration of their borders as well as reduced viability. Statistically significant difference (P<0.05) was observed in number of sprouts when islets were cultured in 3D environment without PPMVF cells.
We have successfully stimulated the formation of peri-islet vessels from human islets with PPMVF cells in 3D matrix support. PPMVF with 3D culture may provide unique avenues to accelerate islet neovascularization following transplantation.