
Pancreas Transplant Alone Outcomes Following Total Pancreatectomy and Islet Autotransplantation Graft Failure
Joseph Sushil Rao1, Srinath Chinnakotla1, David Vock2, Raja Kandaswamy1.
1Solid Organ Transplantation, Department of Surgery, University of Minnesota, Minneapolis, MN, United States; 2Biostatistics, University of Minnesota, Minneapolis, MN, United States
Introduction: Islet auto-transplantation was first performed in 1977, primarily to mitigate brittle diabetes following total pancreatectomy to treat refractory chronic pancreatitis. Total Pancreatectomy and Islet Auto-transplantation (TPIAT) has improved quality of life by not only ameliorating pain but also preventing brittle diabetes in this patient population. However, it has been reported that up to 20% of the patients develop islet graft failure and secondary diabetic complications after TPIAT with some developing hypoglycemic unawareness. Pancreas Transplant Alone (PTA) is an option for patients with TPIAT graft failure, however the outcomes are not widely known. This is the first report to describe the results of PTA in patients with islet graft failure after TPIAT.
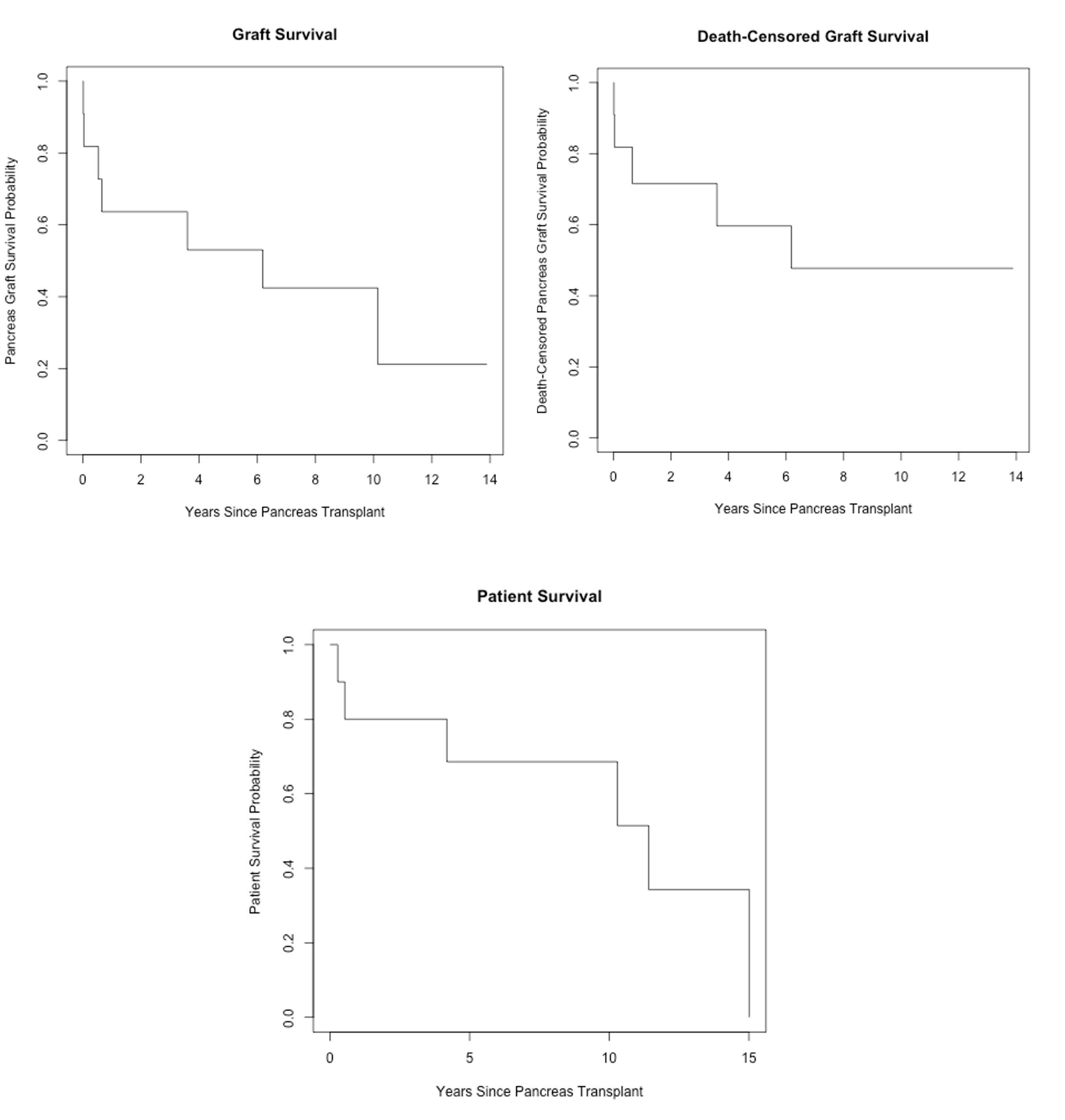
Methods: Using hospital-based records and SRTR database, Chronic Pancreatitis (CP) patients from 1977 to 2008 following TPIAT who developed hypoglycemic unawareness with graft failure and underwent a PTA were included in this study. Recipients of PTA following only TP were excluded from the study. Kaplan Meier (KM) curves for graft survival, death-censored graft survival and patient survival following PTA were plotted. Demographics, etiology of CP, intra-operative notes, post-operative complications, glycemic control/ graft function (HbA1c, c-peptide, hypoglycemic unawareness), rejection episodes and cause of death were documented.
Results: Eight CP patients who underwent TPIAT had graft failure and underwent PTA of which three had a second PTA due graft failure. Four of the eight are deceased due to causes unrelated to diabetes or complications of surgery. KM curves of death-censored graft survival at 5 years show comparable results to modern national cohorts of PTA with 80% 5-year and 70% 10-year patient survival rates.
Two recipients developed Grade 1 and grade 3 Acute Cellular Rejection/ Antibody Mediated Rejection respectively. However, three of the four recipients who are alive partial graft function with positive c-peptide and no hypoglycemic unawareness documented.
Conclusion: PTA can be a treatment option for patients who develop graft failure and hypoglycemic unawareness after TP-IAT, and the results are comparable to PTA for type I diabetics. Larger multicentric studies are needed to confirm these preliminary data.