Impact of insulin therapy in pancreas transplantation donors on graft outcomes: an analysis of the OPTN/UNOS database
Enrique Montagud-Marrahi1,4, Fabio Ausania3, Yiliam Fundora3, Antonio Amor2, Enric Esmatjes2, Joana Ferrer3, Ignacio Revuelta1,4, David Cucchiari1,4, Jordi Rovira4, Mireia Musquera5, Constantino Fondevila3, Fritz Diekmann1,4, Pedro Ventura-Aguiar1,4.
1Nephrology and Kidney Transplantation Department, Hospital Clinic of Barcelona, Barcelona, Spain; 2Diabetes Unit. Endocrinology and Nutrition Department, Hospital Clinic of Barcelona, Barcelona, Spain; 3Hepatobiliopancreatic and Liver Transplant Department, Hospital Clinic of Barcelona, Barcelona, Spain; 4Laboratori Experimental de Nefrologia I Trasplantament (LENIT), Fundació Clínic per a la Recerca Biomèdica (FCRB), Barcelona, Spain; 5Urology Department, Hospital Clinic of Barcelona, Barcelona, Spain
Introduction: Hyperglycemia requiring insulin treatment is frequent in critically ill patients and potential pancreas donors. Information on the impact of donor insulin use on pancreas outcomes is scarce. Thus, we explored the influence of donor insulin use on recipient and pancreas graft survival.
Methods: Retrospective study with 12841 pancreas recipients (either simultaneous pancreas-kidney, pancreas after kidney or pancreas alone) from the OPTN/UNOS registry performed between 2000 and 2017. Multivisceral recipients other than simultaneous pancreas-kidney, those transplants from a donor < 30 kg and recipients with diabetes other than type 1 or 2 were excluded. Insulin donor requirements were defined as the need for any dose of insulin within 24 hours prior to donation. A Propensity Score (Inverse Probability of Treatment Weighting) approach was performed.
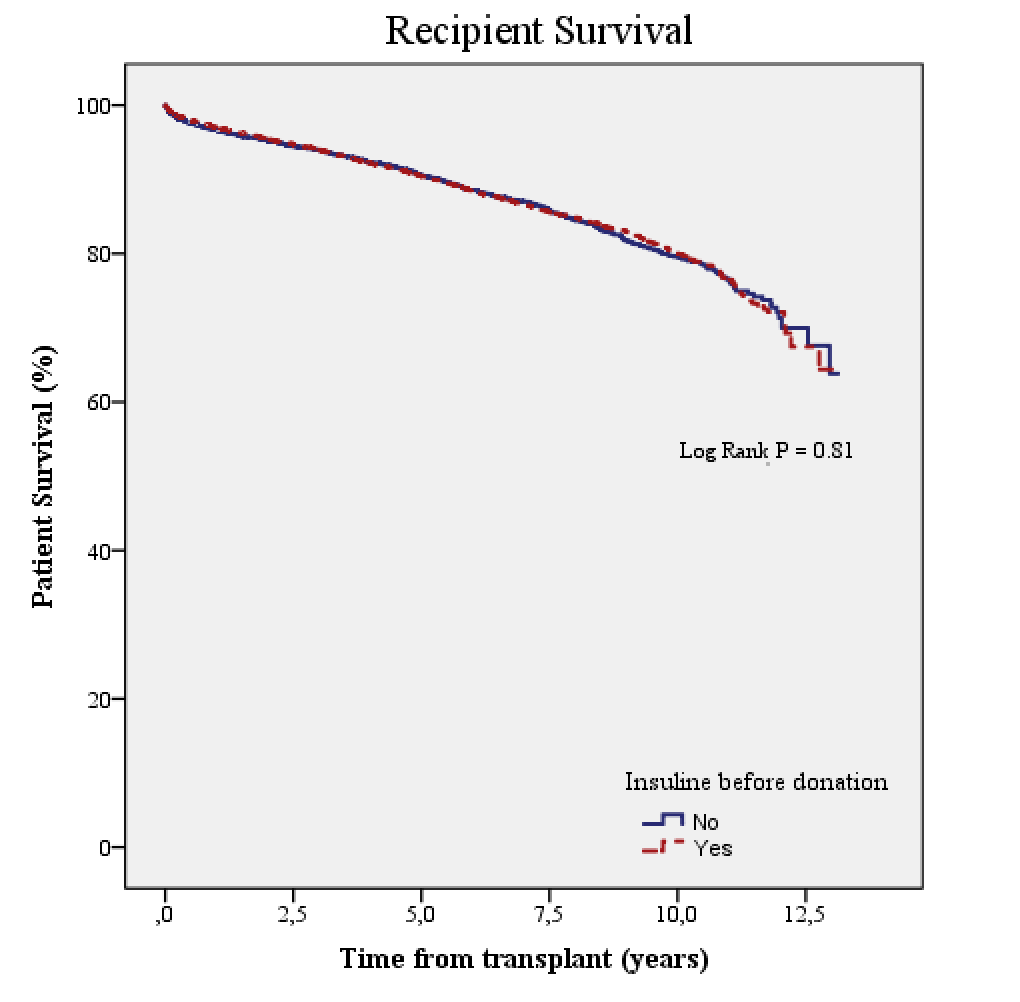
Results: A total of 7765 (60%) patients received a pancreas from a donor with insulin requirements. After inverse probability of treatment weighting on donor and recipient covariates, pancreas graft survival (death-censored) at 1 year was similar between those who received an insulin-requiring donor and the remaining (89% vs 89%, P > 0.05), as well as at 5 and 10 years (78% and 69% vs 79% and 70%, respectively, P = 0.35)(Figure). Donor insulin therapy was not associated neither with an increased risk of recipient death (HR 0.94 [95% CI 0.85-1.04], P = 0.26), pancreas graft failure (HR 1.06 [95% CI 0.98-1.16], P = 0.15) nor any post-transplant complication (HR 1.11 [95% CI 0.98-1.24], P = 0.06).
Discussion/Conclusions: Insulin requirements in a potential pancreas donor is not associated, per se, with an impaired pancreas graft and patient survival. Thus, donors who require insulin therapy may be suitable for pancreas transplantation.
The data reported here have been supplied by the United Network for Organ Sharing as the contractor for the Organ Procurement and Transplantation Network. The interpretation and reporting of these data are the responsibility of the author(s) and in no way should be seen as an official policy of or interpretation by the OPTN or the U.S. Government..