Altered T cell compartment in Type 1 diabetes with End Stage Renal Disease
Shafaq R. Rizvi1, Ravinder Jeet Kaur1, Vikash Dadlani1, Yahya Almodallal2, Corey L. Reid1, Byron H. Smith3, Walter Kremers3, Aleksandra Kukla4, Mark D. Stegall5, Amir A. Sadighi Akha6, Yogish C. Kudva1.
1Division of Endocrinology, Diabetes, Metabolism, & Nutrition, Mayo Clinic, Rochester, MN, United States; 2Department of Medical Oncology, Mayo Clinic, Rochester, MN, United States; 3Department of Biomedical Statistics and Informatics, Mayo Clinic, Rochester, MN, United States; 4Department of Nephrology and Hypertension, Mayo Clinic, Rochester, MN, United States; 5Department of Surgery and Immunology, Mayo Clinic, Rochester, MN, United States; 6Department of Laboratory Medicine and Pathology, Mayo Clinic, Rochester, MN, United States
Introduction: Type 1 Diabetes (T1D) is an autoimmune disease with destruction of beta cells resulting in hyperglycemia and ketoacidosis. A subset of patients with T1D develop End Stage Renal Disease (ESRD) that requires Kidney or/Simultaneous Pancreas and Kidney transplantation (SPK) while those who preserve their renal function require Pancreas Transplantation alone (PTA). Standard immunosuppression therapy does not take into account the individual risk of infection and graft rejection; both are common in these patients after transplantation therefore emphasizing personalized immunosuppression as an unmet clinical need. To achieve this, we undertook more detailed immune studies in wait listed patients.
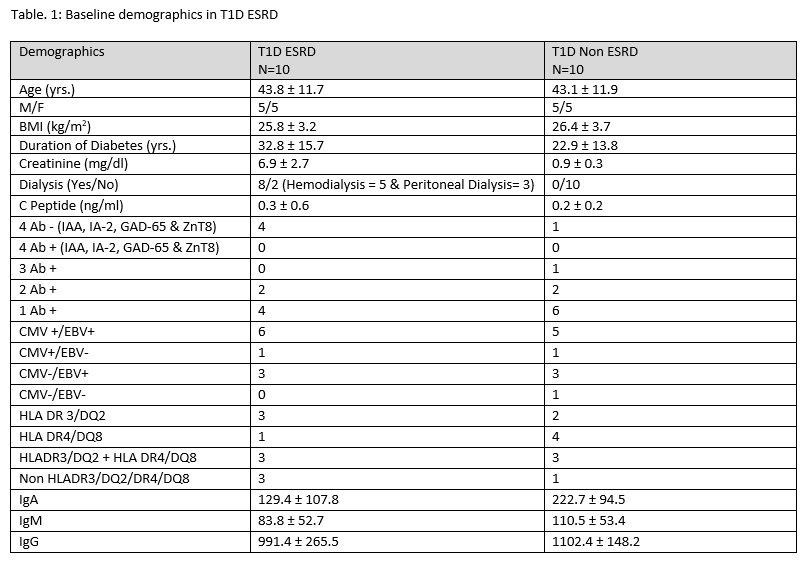
Methods: After IRB approval, we prospectively studied immune cells by flow cytometry in 20 subjects in 2 groups: T1D ESRD, T1D Non ESRD. Each group had 10 subjects who were age and gender matched. We collected baseline C-peptide, Auto antibodies, duration of diabetes, CMV/EBV, HLA and dialysis data. T cell assessments included quantitative immunophenotyping of CD4 and CD8 T cells and their subsets.
Results: Detailed baseline demographics of the two groups are shown under Table 1. T cell subsets showed significant differences (Table 2) in CD4+CD62L-CD27-CD45RO (Tem) cell count (p value: 0.027) and percentages (p value 0.036); Activated CD4 T cell (4+CD25) cell % ( p value: 0.032) , CD8 +CD62L-CD27-CD45RO+ (Tem) cell % (p value: 0.041 )in T1D ESRD Vs. T1D Non ESRD. The increased CD4 and CD8 effector memory T cells (Tem) in the T1D ESRD patients points to a higher likelihood of perhaps ongoing inflammation since active infection was excluded at the screening visit.
Conclusion: Previous studies have reported alterations in the T cell compartment in End Stage Renal Disease Our study substantiates these findings in patients with Type 1 diabetes and ESRD. Future studies with a larger sample size would help to confirm these results. Understanding immune dysfunction better in patients with T1D waitlisted for organ transplantation would contribute to the development of personalized immunosuppression and improve the balance between over and under immunosuppression in individual cases.