Patients report improved diabetes distress after successful pancreas transplantation
Ravinder Jeet Kaur1, Shafaq R. Rizvi1, Corey Reid1, Bradley K. Johnson2, Byron H. Smith2, Shelly K. McCrady-Spitzer1, Walter K. Kremers2, Patrick Dean3, Aleksandra Kukla4, Mark D. Stegall3, Yogish C. Kudva1.
1Division of Endocrinology, Diabetes, Metabolism, & Nutrition, Mayo Clinic, Rochester, MN, United States; 2Department of Biomedical Statistics and Informatics, Mayo Clinic, Rochester, MN, United States; 3Department of Surgery and Immunology, Mayo Clinic, Rochester, MN, United States; 4Department of Nephrology and Hypertension , Mayo Clinic, Rochester, MN, United States
Introduction: Type 1 Diabetes (T1D) is associated with increased severe hypoglycemia, decreased hypoglycemia awareness and diabetic ketoacidosis. These comorbidities are associated with decrease quality of life and increase diabetes related distress in T1D patients with uncontrolled diabetes. Some of these patients are evaluated for Pancreas Transplantation (PT) but limited data exist about diabetes related distress after PT. Therefore, we prospectively studied diabetes related distress reported by patients with Type 1 Diabetes (T1D) after Pancreas transplantation (PT) over a period of one year.
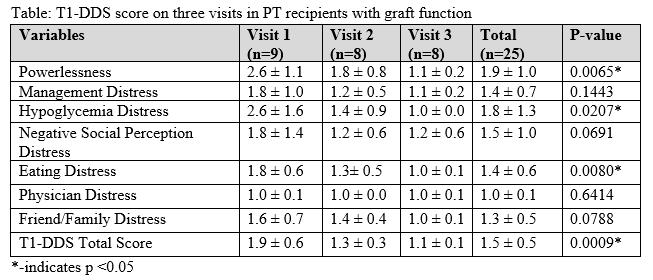
Methods: Eleven PT recipients (6 pancreas transplantation alone, 4 simultaneous pancreas kidney transplantation and 1 Pancreas after kidney), were enrolled within a month of PT and completed 3 visits (V1, V2 & V3 at 4 weeks, 4 months and 1 year). At each visit, participants completed Type 1-Diabetes distress scale (T1-DDS) reporting distress related to diabetes. T1-DDS contains 28 questions, with each item rated on a 6-point scale from “(1) not a problem” to “(6) a very significant problem”. Overall distress score, as well as scores for individual subscales are rated on scale of 1-6 on the average response on all the items. An average score below 2, indicates little or no distress, score between 2.0-2.9, indicates moderate distress and score above 3 indicates high distress. We analyzed insulin independent and insulin dependent (partial graft failure) participants separately. A statistical analysis was done using a linear mixed effects model to obtain a p-value.
Results: PT recipients were 45.5 ± 13.8 years old, 10 F, duration of T1D 28.3 ± 15.1 years with 29 ± 17.4 days interval from PT. Laboratory results showed HbA1c (%) of 6.3, 5.4 and 5.4, fasting plasma glucose (mg/dL) of 87.4, 104.8 and 91 and C-peptide (ng/ml) of 4.7, 3.1 and 2.4 on V1, 2 & 3 respectively. Two participants out of 11 had partial graft failure and became insulin dependent. During V1, insulin independent participants (n=9) showed moderate distress related to powerlessness and hypoglycemia distress subscales, which significantly improved by V3 (Table) with little or no distress at all along with improvement in eating distress subscale from V1. There was significant improvement in total diabetes distress score (p 0.0009) in all insulin independent participant over 1 year. Two participants who became insulin dependent due to partial graft failure did not show significant improvement in diabetes distress score from V1 to V3 except for hypoglycemia distress subscale (V1: V2: V3=3.5: 3.4: 2.9, p 0.0372) which improved from high distress to moderate distress.
Conclusion: PT recipients reported little or no diabetes related distress over a period of 1 year with good graft function. These results are important for counselling and decision making for T1D patients who are struggling with poor quality of life and are looking for PT as an option in future.